by Donna Johnson
PAD Journey Part I: Diagnosis
Have you heard of Peripheral Artery Disease, otherwise known as PAD for short?
Yea, me neither until the diagnosis turned our world upside down on May 6, 2021.
I’m sharing our journey for awareness since this disease is seldom heard of, but often misdiagnosed.
It’s usually brushed off by doctors and individuals as old age, poor circulation or neuropathy.
I say “our” journey, because this impacts me as much as Mark, my husband.
Our lives are forever changed as a result of PAD.
PAD is a plaque build-up in the arteries of the peripherals (arms, brain, legs), mainly the legs. It’s just like coronary artery disease (heart attack)or carotid artery disease(stroke) except the plaque build-up is in my legs.
PAD is a chronic illness in which there is currently no cure, but long-term management is possible.
So, what are some of the risk factors for PAD, you ask?
* Family History – Cardiovascular Disease/PAD
* Obesity
* Smoking (current or past)
* High Cholesterol & Hypertension
* Chronic Kidney Disease
* Age – over 50
* Pre-Diabetes, Diabetes
For me the primary cause of my plaque build up was attributed to smoking. I also had risk factors of family history, elevated cholesterol, and over 50 against me. However, the doctor attributes smoking as the primary cause of my plaque build-up.
PLEASE NOTE: I stopped smoking 20 years ago. So I’ve had plaque building in my legs, unnoticed and undetected, for a very long time!
The chief challenge in the management of peripheral arterial disease is retooling of the health system to focus on proactively identifying patients with PAD and taking the enormous opportunity and responsibility to refine and aggressively manage the atherosclerotic risk factors in these patients.
Prevention screening for PAD, just like mammograms, colonoscopies, and other prevention screening is key to early diagnosis!
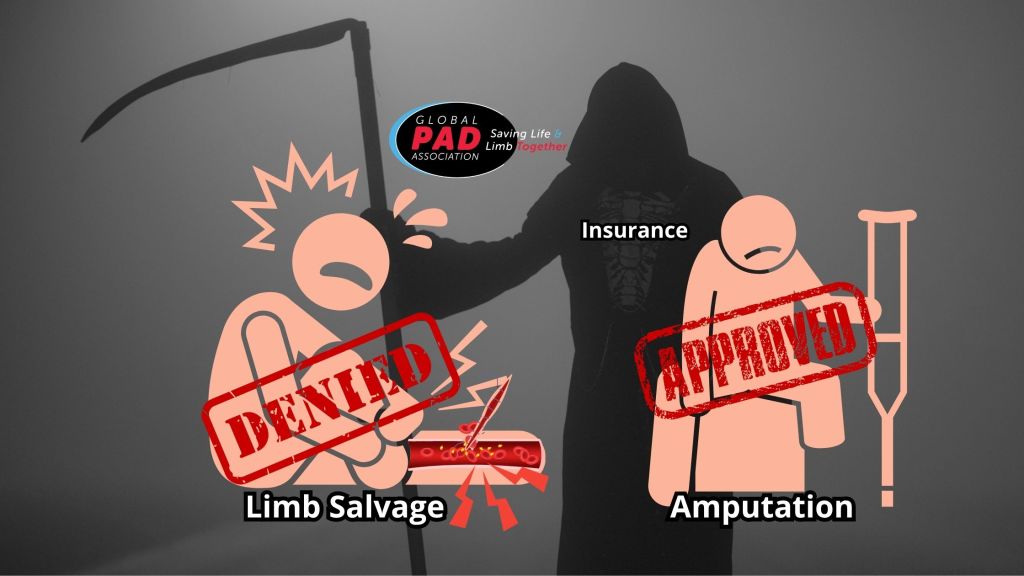
Early diagnosis is key because PAD can be managed with Pharma, lifestyle modifications (Diet, Exercise, etc.) and/or minimally invasive surgical treatments. Advanced stages may require more invasive procedures such as bypass and amputation.
The good news is that I can play a major role in my prognosis. I can slow disease progression by getting to the root cause of what’s damaging my arteries, making critical lifestyle modifications, and timely treatment.
If you go on to Dr. Google, your online research will reveal a 5-year mortality for PAD patients.
But take a deep breath because that older research does not take into consideration early diagnosis and newer interventional approaches, which significantly improve the prognosis.
Some patients in our network are walking 20 years after diagnosis with the right doctor & treatment plan.
I intend to be ONE of those patients.
That’s even with long calcified areas in my arteries that some vascular doctors would consider the ‘Achilles Heal’ of their practice.
I had a 95% artery blockage hip to knee and 100% blockage knee to ankle in the left leg.
I had an 80% artery blockage hip to knee and 100% knee to ankle in the right leg.
How do those blockages translate into how I feel?
My symptoms (intense leg, calf & foot pain, cramping, numbness) became noticeable March 8, 2021 and it took until May 6, 2021 for a final diagnosis. Simple walking became unbearable and stairs or inclines impossible without resting every few steps.
This is called “lifestyle limiting claudication.”
Claudication is the cramping you feel while you walk when the artery blockages are restricting blood flow carrying critical nutrients, including oxygen, to your muscles and nerves trying to work.
With “lifestyle limiting claudication,” the crampiness eases up when you stop walking for a few minutes.
The irony is that the more you push through that cramping, the better you should feel over time (Just don’t overdue it! Know your threshold).
It’s because your body starts to build a ‘natural bypass’ around the blockages the more your body demands additional blood flow your main arteries can’t provide.
So, when you feel that cramping, it’s actually the trigger for your body’s collateral network of vessels to kick into gear and help keep blood flowing to supply your lower legs and feet.
It just takes time to start seeing your extra effort translate into symptom relief.
I’ve read in the Global PAD Association’s “How To Walk” publication, that it sometimes takes 6-8 weeks, in fact.
Make sure to have that conversation with your vascular doctor to get started with the best walking program for you.
PAD Journey Part II: Advanced Treatment
I have a talented interventional vascular specialist, which is critical to taking steps to slow disease progression and save my toes, feet, and legs!
Not all vascular doctors have the same skills, and although they tell you they treat PAD, it’s important to interview them using important criteria here, to figure out if they are the best for your situation.
Again, I don’t want to be a statistic within the 5-year mortality category, nor do I want to be forced to amputate any one or part of my limbs.
Neither do you!
That’s why you have to get down to the tools and methods they use to open arteries if walking and medicine doesn’t work to improve your symptoms.
The key for me was having my vascular doctor just get enough blood flow so I wouldn’t feel horrible leg cramps the moment I started walking and could walk more.
He did an angioplasty (inflated a balloon in my artery to push plaque aside) on my left leg on June 16, 2021 and my right leg on July 9, 2021.
He made sure I was signed up for an 18-week cardiac rehab, specifically for PAD patients on July 20, 2021, to make sure I would do my part in the process.
It’s known as Supervised Exercise Therapy (SET)when it’s specifically for PAD.
This is a new program, which began in 2021, that my Interventional Cardiologist was instrumental in getting started at the hospital. I’m fortunate to have medically supervised rehab specifically for PAD patients available to me. If I was diagnosed any sooner, this would not have been an option for me. I’m thankful to have it now!
The end game of this program is simple: To increase the amount of time I can walk without pain, maximize the time between angioplasty procedures by exercising, walking, lifestyle changes including diet, learn to live and adjust to a new normal that doesn’t take for granted life’s simplest things like using my legs.
It will be considered a “win” if I can progress to the point where 80% of my daily activities involving my legs can be performed pain free.
PAD Journey Part III: Mental Impact
Instead of asking myself how this happens to someone who, over the last 15 years has focused on healthier living, I thank God every day that I did focus on making fit happen.
I had already quit smoking long before my PAD Diagnosis (As mentioned before).
I was already eating healthier.
And I had being doing CrossFit, a.k.a. functional fitness, which I believed saved my legs! My vascular system compensated for the reduced blood flow by forming those alternative routes, called collateral vessels, which bypassed my blockages and kept me from needing a doctor a lot longer. The development of these collateral pathways were created by doing CrossFit over the years. It turns out that the only thing that fueled my oxygen and blood-starved legs were collateral pathways created by years of intense exercise. Without these collaterals, I would have lost my legs years ago.
I truly believe CrossFit literally saved my legs!
I’m also so grateful for that and so thankful for advancements in medical science that gives me so much hope for the future.
I’m grateful that God walks beside us in the battle and encourages us to believe in the possibilities.
I have accepted that life is different now with PAD.
Priorities do shift when your world changes.
Things that seemed important before, take a backseat to your health.
But focusing on improving my health gives me more time to do other things I still want to continue to enjoy in life, including family and friends.
It’s not always easy to keep that positive energy and hope alive.
Today, I still struggle to walk, despite all of my efforts.
But I’ve come so far!
I just don’t let the cramping hold me back.
I do keep praying that it will get easier as time goes on.
In the short-term, they key for my mental health is to keep celebrating the small wins we strive to recognize each and every day.
PAD Journey Part IV: Moving Forward
The biggest win so far was in 2023, when I was finally able to stabilize the arteries in my legs and stop the vicious cycle of angioplasty every six months.
I’ve just surpassed 14 months without an intervention, which is amazing considering I couldn’t go 6 months without one the first two years of being diagnosed.
Overall, I credit my success to several key factors:
1. Being my own medical advocate
2. Doing my own research, research, and more research
3. Reading Preventing and Reversing Heart Disease by Dr Caldwell Esselstyn
4. Walking 10,000 steps a day
5. Exercise and Strength training 3 times a week 6
6, Eating healthy plant-based, whole foods
7. Controlling my LDL cholesterol and keeping it below 50 through medication played an important role in that, coupled with diet and rigorous daily exercise. (It helps that my Interventional Cardiologist is a nationally recognized lipidologist. Through his expertise and support, I’ve been able to stabilize the progression of the PAD and even reverse it just a little bit.)
8. And most importantly, never losing faith!
I post this journey for general awareness of a little know, misdiagnosed, silent disease: Peripheral Artery Disease (PAD). This diagnosis will not steal my joy or love of life. It will change our lives, but it will not control my life.
Hope is found in each footstep forward!
#PADWarrior #PADawareness #strongerthanPAD #makefithappen


Leave a comment